Trust Impact Calculator
How Trust Affects Public Compliance
The article shows that when public trust in health authorities is high, compliance with health measures increases by 23-47%. This tool calculates the potential impact of trust levels on compliance rates.
Estimated Compliance Impact
When a disease starts spreading fast, people don’t just want numbers. They want to know: Can I trust this? Can I believe what they’re telling me? Will this advice actually keep me and my family safe?
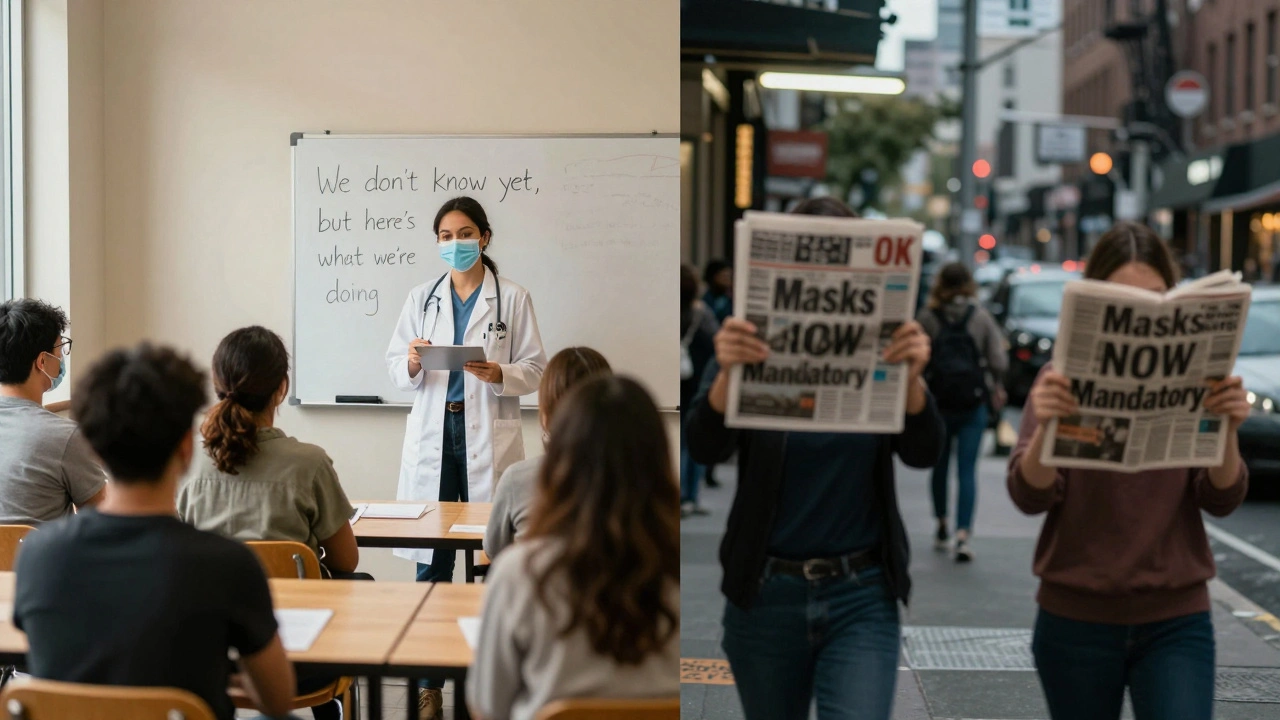
During the COVID-19 pandemic, we saw how quickly trust can crumble. One day, masks were unnecessary. The next, they were mandatory. Then, guidance changed again. People didn’t just get confused-they got angry. And when anger takes over, even the best science doesn’t matter. That’s the real danger in an epidemic: not the virus itself, but the collapse of public trust.
Trust Is the Real Vaccine
Dr. Sylvie Briand from the WHO called trust the "critical vaccine" in health emergencies. It’s not a metaphor. Studies show that when people trust the source, they’re 23% to 47% more likely to follow health advice-whether it’s staying home, getting tested, or wearing a mask. That’s not a small difference. That’s the difference between controlling an outbreak and watching it spiral.
Compare Finland’s approach to the U.S. during the same pandemic. Finland’s health institute, THL, sent out clear, daily updates. They didn’t hide uncertainty. They said things like, "We don’t know yet, but here’s what we’re doing to find out." Their Twitter account, @THLfi, got a 4.8 out of 5 satisfaction rating. Meanwhile, the CDC’s shifting guidance on masks led to widespread frustration. On Reddit alone, 61% of negative comments blamed "changing rules" for eroding trust.
It’s not about being perfect. It’s about being honest. People can handle bad news. They can’t handle being lied to-or being kept in the dark.
The Seven Pillars of Effective Risk Communication
There’s a science to this. After decades of mistakes and lessons learned-from HIV/AIDS to Ebola to COVID-19-experts have identified seven non-negotiable elements of effective risk communication during epidemics.
- Timeliness: Information must come out within 24 hours of a new risk being confirmed. Finland’s THL did this consistently. Delayed messages breed rumors.
- Transparency: 89% of trusted communications openly admitted uncertainty. Saying "We’re still learning" builds more credibility than pretending to have all the answers.
- Consistency: Messages across government agencies, hospitals, and media had to match 95% of the time. Contradictions destroy trust faster than silence.
- Accessibility: Information had to be available in all major languages spoken in the community. In multicultural cities, this isn’t optional-it’s survival.
- Actionability: People need clear, simple steps. "Wash your hands" is good. "Practice enhanced hygiene protocols" is not. The best messages tell people exactly what to do, when, and why.
- Two-way engagement: Authorities didn’t just broadcast. They listened. Systems in Finland and South Korea monitored over 500,000 social media posts daily to catch rising fears and misinformation before they spread.
- Trust indicators: Messages that named the expert behind them-"Dr. Maria Lopez, Epidemiologist at THL"-were 92% more trusted than generic government statements.
These aren’t suggestions. They’re the baseline for any system that wants to work during a crisis.
Why Some Countries Got It Right-and Others Didn’t
Not all countries had the same resources. But the difference wasn’t just money. It was culture, history, and pre-existing trust.
Uganda’s Ebola response succeeded because they didn’t start from scratch. They used existing community health workers-people already trusted in villages. Compliance hit 92%. In places without those networks, it was only 67%.
South Korea’s real-time exposure notification app during MERS had 91% public compliance. But when they tried the same app during COVID-19 in the U.S. and Europe, 63% of people refused to use it-because of privacy fears. The tech was the same. The trust wasn’t.
Even the best communication model fails if the public doesn’t believe the messenger. The WHO’s RCCE framework works better in diverse, collectivist societies. The CDC’s CERC model, with its "myth vs. fact" approach, works better in highly polarized places like the U.S.-but only if it’s not drowned out by political noise.
When political leaders contradicted health experts, trust dropped. In the U.S., government communications averaged 61% public trust during COVID-19. The WHO’s global messages hit 83%. Why? Because people saw WHO as less tied to local politics.

The Cost of Getting It Wrong
Bad communication doesn’t just confuse people. It makes them sicker.
Conspiracy theories don’t just spread-they amplify fear. Studies show that exposure to false claims about vaccines or government cover-ups increases perceived risk by 42% and cuts trust in authorities by 31%. That’s not a rumor. That’s a measurable spike in public panic.
And fixing broken trust is expensive. Harvard research found that repairing trust after a failure takes 3.7 times more effort than maintaining it. You can’t just issue a correction. You need five steps: acknowledge the mistake, explain why it happened, correct the record, take accountability, and show how you’ll prevent it again.
Look at the UK’s early pandemic briefings. Public satisfaction ratings were 2.3 out of 5. Why? People saw political interference. They didn’t trust the messenger, so they ignored the message-even when it was correct.
The financial cost is just as real. The global risk communication market hit $1.24 billion in 2023. High-income countries spent heavily. Low-income nations? Only 47% have basic systems. The WHO estimates a $3.2 billion gap to fix that by 2025. That’s not a charity issue. It’s a global security risk.
What Works in Practice
Here’s what real-world success looks like:
- Finland’s THL: Monitored 1.2 million social media interactions weekly. Used AI to detect trust erosion patterns with 87% accuracy. Published weekly "myth-busting" videos. No jargon. No fluff.
- Singapore: Took 22 months to build its system before the pandemic. Integrated risk communication into every public health department. Result? One of the lowest death rates per capita in Asia.
- Canada’s EXCALIBUR: Uses AI to scan 500,000 social posts daily in 47 languages. Detects emerging rumors 72 hours before traditional surveys. Proven in the 2023 Mpox outbreak.
These systems didn’t happen by accident. They required teams: epidemiologists, communication specialists, behavioral scientists, and community liaisons. WHO recommends 5 to 15 specialists per million people. Most countries don’t have that. But even small steps help.
Start with transparency. Start with clarity. Start with listening.

What You Can Do Now
You don’t need a national budget to build trust. If you’re a local health official, a school administrator, or even a community leader, here’s how to start:
- Admit when you don’t know. Say it out loud. People respect honesty more than false confidence.
- Use plain language. No acronyms. No jargon. "Flu-like symptoms" instead of "respiratory syndrome with fever and myalgia."
- Identify trusted local voices. Clergy, teachers, neighborhood leaders-they have more influence than any press release.
- Monitor social media. Even a volunteer team can track trending concerns on Facebook or Nextdoor. Respond quickly.
- Repeat key messages. People forget. Say it again. And again. In different ways.
Trust isn’t built in a press conference. It’s built in small, consistent, honest interactions over time.
What’s Next?
The WHO’s 2024-2028 strategy now requires countries to measure public trust weekly during outbreaks using a standardized 12-question scale. That’s a big shift. For the first time, trust isn’t just a nice-to-have-it’s a metric.
And AI is changing the game. Systems like EXCALIBUR can predict where panic will flare before it happens. But technology alone won’t fix broken trust. Only honest, human communication can do that.
The next epidemic is coming. The question isn’t whether we’ll be ready. It’s whether we’ve learned how to speak to people-not at them, but with them.
Why does public trust matter more than scientific accuracy during an epidemic?
Science tells us what’s happening. Trust tells people whether to act on it. A perfectly accurate message that no one believes won’t stop a single infection. Studies show that when trust is high, public adherence to health measures increases by 23% to 47%. That’s why WHO calls trust the "critical vaccine." Even the best data fails if people don’t believe the source.
What’s the biggest mistake health officials make in risk communication?
Trying to sound perfect. When officials pretend they have all the answers-even when they don’t-it backfires. People notice when information changes. If they’re told one thing today and the opposite tomorrow, they assume they’re being lied to. The most trusted messages include phrases like, "We’re still learning," or, "We don’t know yet, but here’s what we’re doing." Transparency about uncertainty builds more credibility than false certainty.
Can social media be used to build trust, or does it just spread misinformation?
It can do both. The key is active listening. Finland’s THL monitored over a million social media interactions weekly. They didn’t just post updates-they watched what people were worried about. Then they responded directly. When people see their concerns being heard and addressed, even in a comment section, trust grows. Passive broadcasting creates distance. Two-way engagement builds connection.
Why do some communities respond better than others to the same health messages?
Pre-existing trust matters. Uganda’s Ebola response worked because they used community health workers-people already trusted in villages. In places without those networks, compliance dropped. It’s not about the message. It’s about the messenger. If a community already trusts its local leaders, they’re far more likely to follow advice-even if it’s hard. That’s why building relationships before a crisis is critical.
Is risk communication expensive to implement?
Yes, but not as expensive as a failed response. The WHO recommends 5 to 15 specialists per million people, including epidemiologists, communicators, and community liaisons. High-income countries spend heavily. Low-income nations lag behind, with only 47% having basic systems. The global funding gap is $3.2 billion by 2025. But the cost of inaction is higher: uncontrolled outbreaks, overwhelmed hospitals, and lost lives. Investing in communication saves lives-and money-in the long run.
Can AI replace human communicators in risk communication?
No-but it can make human communicators much more effective. Canada’s EXCALIBUR system scans half a million social posts daily to detect rising fears and false claims 72 hours before traditional surveys. That gives officials time to respond before panic spreads. But AI can’t say, "I’m sorry we got this wrong," or explain why a policy changed. Only humans can build trust. AI handles speed and scale. Humans handle empathy and accountability.
What’s the most important thing a local official can do right now to prepare?
Start listening. Identify who your community already trusts-teachers, faith leaders, local business owners. Build relationships with them now, before a crisis hits. Practice speaking plainly. Record short, clear videos explaining simple health steps. Test your messages with real people. Don’t wait for an outbreak to learn how to communicate. Trust is built over time, not in a press release.